Legislative framework
In the context of consent and authorisation
On this page:
The legislative framework for donation in England, Wales and Jersey is that of a soft opt out system of consent, while Scotland (authorisation), Northern Ireland, Guernsey and the Isle of Man are currently in the process of moving to this system.
In England, Wales and Jersey a soft opt-out system means that unless an individual records a decision on the Organ Donation Register (ODR), in writing or verbally expresses that they either wanted to or did not want to be an organ donor, they are considered as not having an objection to donation after their death and their consent is deemed.
To support this change, the NHS Organ Donor Register (ODR) was modified in July 2015 to allow anyone in the UK to register a decision to donate, to register a decision not to donate or to nominate a representative to make a decision for them after their death. Although the soft opt-out system of consent only applies in England, Wales and Jersey, anyone in the UK can now register a decision not to donate. The appointment of a nominated representative has no legal standing in Scotland and an individual in that position would not be able to undertake that role.
Countries or territories where deemed consent applies
The Human Tissue Act 2004, the Human Transplantation (Wales) Act 2013, Human Transplantation and Anatomy (Jersey) Law 2018 and The Deemed Consent (Organ Donation) Act 2019 legislate for deemed consent as a lawful and appropriate form of consent within each country or territory’s borders.
Steps for exploring consent for organ donation in Wales, Jersey and England
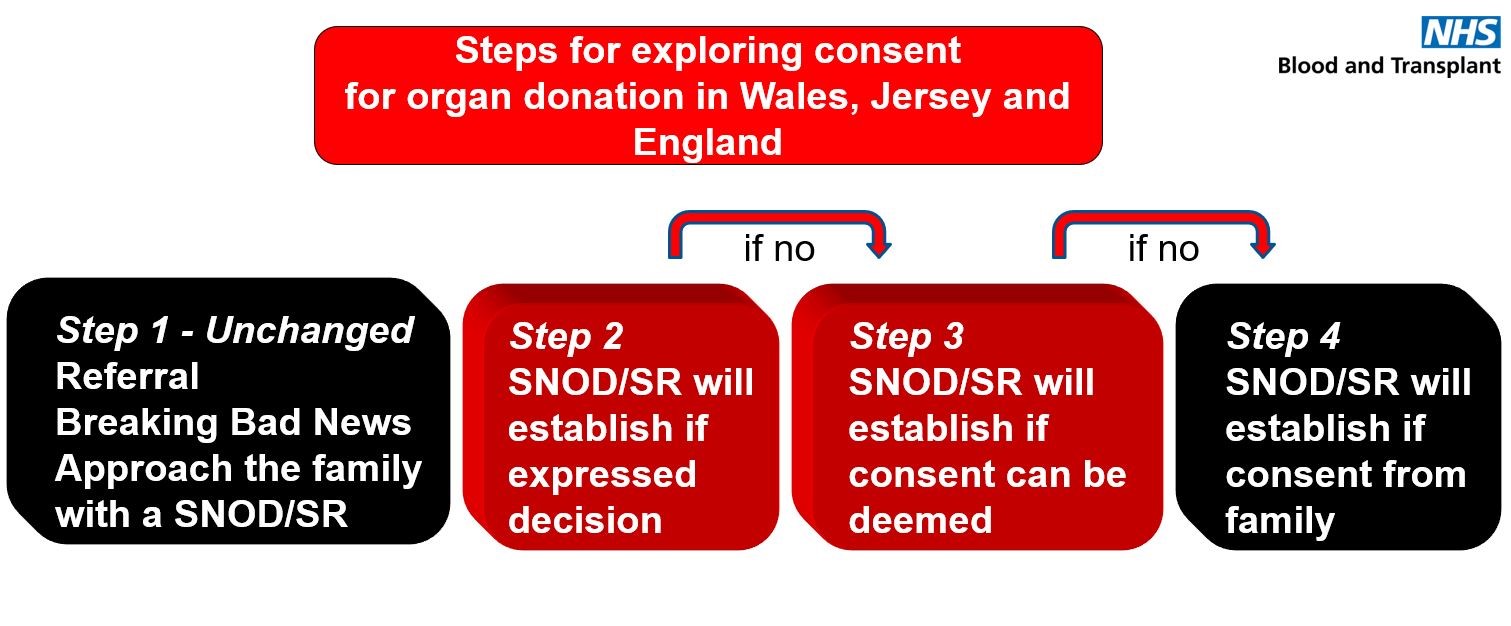
Step 1 – referral, breaking bad news, approach the family with a SNOD/SR
This is a usual and established practice where a potential donor is referred to the Organ Donation Services Team, the family are told that their loved one has died / will die imminently and the Specialist Nurse for Organ Donation (SNOD) or Specialist Requester (SR) is on hand to support the family through end of life care.
Step 2 – SNOD/SR will establish if expressed decision
The last know decision of the patient takes primacy in all conversations where donation is discussed. To that end, the SNOD/SR will establish if the potential donor had made a decision in life about donation, whether that’s to be a donor or not.
This discussion will include if the potential donor had registered their decision on the ODR, in writing (eg their will), or had verbally expressed a donation decision. If there is a decision in place, this is the one that should be followed and the family are expected to support that.
Step 3 – SNOD/SR will establish if consent can be deemed
Where there is no decision in place, the SNOD/SR will seek to establish if deemed consent can apply. The inclusion criteria that must be met for deemed consent to apply are:
- Over 18 years old
- Are ordinarily resident in the country of death
- Had mental capacity during the 12 months leading up to their death.
Only in these circumstances can deemed consent be applied.
Step 4 – SNOD/SR will establish if consent from family
If deemed consent cannot be applied as the patient triggers an exclusion for deemed consent, then the family will be asked to make a decision on behalf of their loved one, based on their knowledge of the patient’s values, character and beliefs.
Countries or territories where opt out legislation has not been introduced
Scotland, Northern Ireland, Guernsey and the Isle of Man continue to work under opt-in legislation, although each have put forward plans to change to an opt out system. Scotland will be introducing the Human Tissue (Authorisation) (Scotland) Act 2019 on March 26th 2021, which will see deemed authorisation become a lawful and appropriate mode of obtaining authorisation.
As the process of legislation continues through the appropriate governmental systems and operational teams are readied for the forthcoming changes, organ donation will continue to be delivered as it always has.
Steps for exploring consent / authorisation for organ donation in Northern Ireland, Scotland, Guernsey and Isle of Man
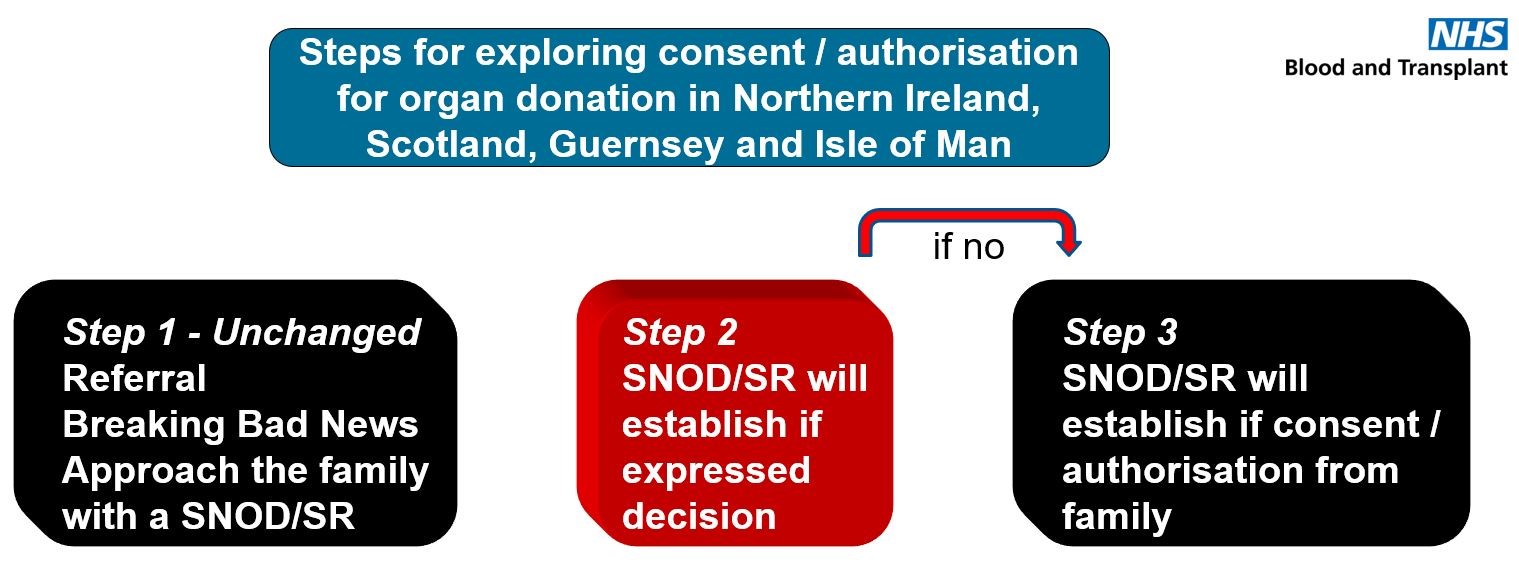
Step 1 – referral, breaking bad news, approach the family with a SNOD/SR
Donor is referred to the Organ Donation Services Team, the family are told that their loved one has died / will die imminently and the Specialist Nurse for Organ Donation (SNOD) or Specialist Requester (SR) is on hand to support the family through end of life care.
Step 2 – SNOD/SR will establish if expressed decision
The last know decision of the patient takes primacy in all conversations where donation is discussed. To that end, the SNOD/SR will establish if the potential donor had made a decision in life about donation, whether that’s to be a donor or not.
This discussion will include if the potential donor had registered their decision on the ODR, in writing (eg their will), or had verbally expressed a donation decision. If there is a decision in place, this is the one that should be followed and the family are expected to support that.
Step 3 – SNOD/SR will establish if consent from family
If no decision can be established, then the family will be asked to make a decision on behalf of their loved one, based on their knowledge of the patient’s values, character and beliefs.
The role of the family
There is no legal provision in any of the Acts for family members to veto an individual’s decision, be this to be a donor or not. The law in England/Wales/Jersey is permissive and allows donation to proceed, however, the law does not mandate that donation must proceed and as such the family are consulted with.
Scottish legislation requires families to complete a retraction form should they seek to overrule a loved one's decision to be a donor.
It is important to understand that although the Acts give precedence to the decision of the patient, when those decisions cannot be established, and in England, Wales and Jersey when decisions cannot be deemed (and in the absence of a nominated representative (not Scotland)), authority for decision making passes to the individual in the highest qualifying relationship / nearest relative to the patient.
Careful thought should be given to how donation is raised and which legislative framework applies, taking into account the specific circumstances of the patient and family.
Approaches that place exclusive emphasis upon honouring the decision of an individual may lead families to erroneously conclude that donation should not happen when such decisions cannot be established, even though they then have the legal authority to consent to /authorise it.
Donation from children
A child is considered a person under the age of 18 years. In Scotland, the definition of a child varies in different legal contexts, but statutory guidance which supports the Children and Young People (Scotland) Act 2014, includes all children and young people up to the age of 18.
All UK organ donation legislation recognises the validity of the decisions of competent minors therefore where a child has recorded a decision and is deemed competent to have made that decision it should be considered no different than that of an adult.
Where the decision of the child is not known or the minor was not considered competent to deal with the issue, consent / authorisation passes to a person with parental responsibility, or if there was no one with parental responsibility directly prior to the child’s death or they are incapacitated, to an individual in a qualifying / nearest relationship.
There is no age restriction for self-registration or self-withdrawal from the register (excluding Scotland). A parent can also register a child for whom they have parental responsibility; alternatively, a child can register themselves.
Scotland
In Scotland, the definition of a child varies in different legal contexts but under the Human Tissue (Scotland) Act 2006 a child is considered to be aged under 16 years.
The framework of the 2006 Act does not permit a child aged under 12 years to make an express authorisation or opt out declaration in respect of donation. In the case of a child aged under 12 years, authorisation for donation may be provided by a person with parental responsibility for the child.
Children aged over 12 years can self-authorise (or opt out of donation on the ODR or in writing) and this decision should be considered no different from that of an adult, if there is no decision then authorisation must be taken from the person with parental responsibility (unless common calamity). The person giving authorisation must be over 16 years of age themselves (to authorise someone else), unless they themselves hold parental responsibility for that child.
