Paediatric care
On this page
Paediatric Organ Donation
The Organ Donation Task Force (2008) saw an associated 50% increase in donation within the overall population, this was not reflected in paediatrics where rates have remained relatively static over the last 10 years.
Number of deceased paediatric (less than 18 years) donors, transplants and active transplant list in the UK, 1 April 2013 – 31 March 2023
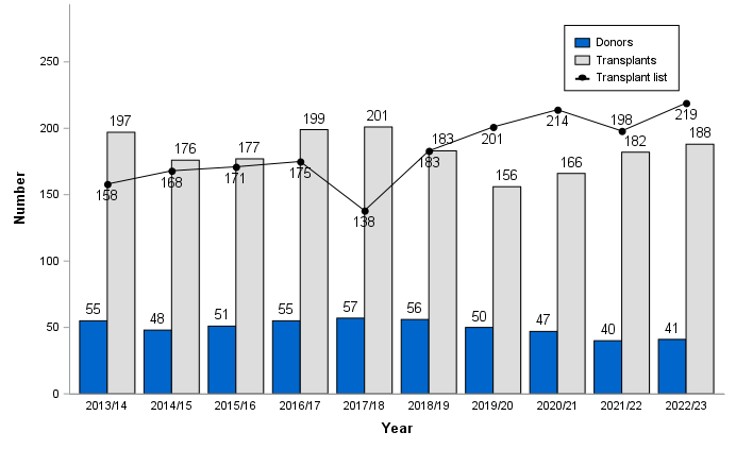
Waiting list figures at the 31 March 2020 do not accurately reflect the need for an organ transplant due to the COVID-19 pandemic. Different practices have been established across the UK and across organ groups with regards to waiting list management. Due to this, a snapshot of the waiting list at 29 February 2020 is used to better reflect activity near the end of 2019/20.
There are 26 Paediatric Intensive Care Units (PICU) across the country with around 13,000 children admitted each year; nearly half of those being under one year of age. It is relatively rare for children to die in a Paediatric Intensive Care Unit; compared to adults admitted to intensive care, the survival rates for paediatric patients are much higher, with over 95% survival. (source: Paediatric Intensive Care Medicine - Royal College of Paediatrics and Child Health).
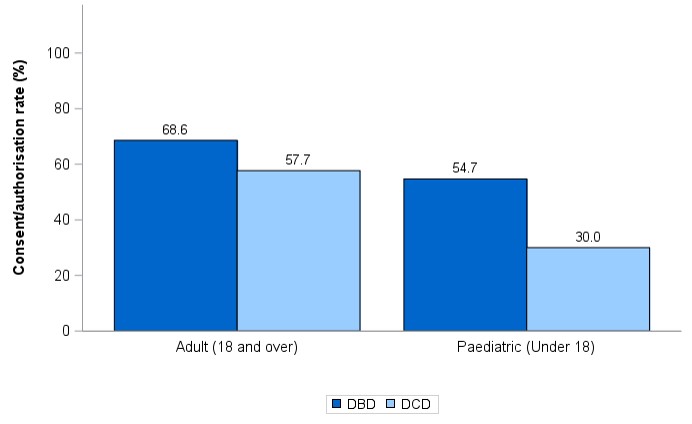
The UK consent rate for paediatric DCD organ donation falls below the national average for the adult population.
DBD and DCD consent/authorisation rates by age group and donor type, 1 April 2022 – 31 March 2023
End of life care guidance and practice does differ from adult practice and care of the family unit as a whole is a core principle.
In line with strategy recommendations we are working to ensure that where organ donation is possible families are given the opportunity to consider it, along with other possible options for end of life care. We aim to work towards a culture of choice in end of life care that supports organ donation and works in parallel with PICU and palliative care practices.
Find out about our update to national practice (April 2023).
Useful Resources
- Paediatric NODC Benchmarking Data - April 2021 - March 2023 (PDF 666KB)
- Paediatric NODC Benchmarking Data - April 2020 - March 2022 (PDF 609KB)
- Paediatric NODC Benchmarking Data - April 2019 - March 2021 (PDF 600KB)
- Paediatric NODC Benchmarking Data - April 2018 - March 2020 (PDF 597KB)
- Paediatric NODC Benchmarking Data - April 2017 - March 2019 (PDF 634 KB)
- Paediatric NODC Benchmarking Data - April 2016 - March 2018 (PDF 1.2MB)
- Paediatric NODC Benchmarking Data - April 2015 - March 2017 (PDF 523KB)
- PICS Standards
- Annual report on donation and transplantation in paediatric patients
External links
Paediatric Donation after Circulatory Death
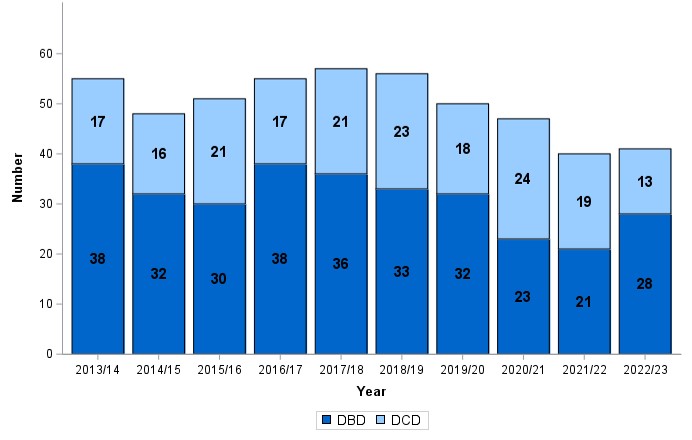
Donation following Circulatory Death (DCD) in children has increased in line with adult trends, becoming a significant area of donation. In part a contribution to this increase has been advances in DCD donation in very small infants and neonates which has been noted since 2012.
The reason for the increase in donation from small infants has been attributed to advances and development of techniques in en-bloc renal transplantation, development of hepatocyte transplantation from this age group and media coverage which has enabled families to feel empowered to come forward to seek information on the option of organ donation.
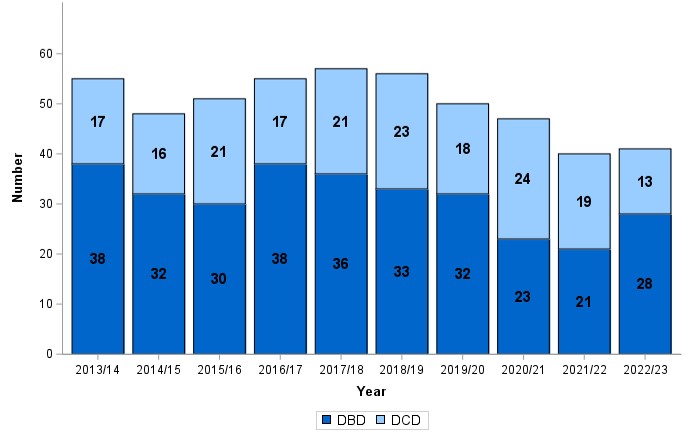
Donors aged less than 18 by donor type, 1 April 2013 – 31 March 2023
In the absence of clear ethical framework for donation in paediatrics UK Donation Ethics Committee published a position paper in June 2015 to examine ethical issues that may arise taking into account how practices in end of life care in children can affect decision making. It provides a framework for decision making while respecting any known wishes or beliefs the child may have had.
The specialist nurses receive specific training to increase awareness and understanding of paediatric and neonatal systems to ensure they are well equipped to support and facilitate donation in this environment. In addition to this teams should ensure robust policies are available in all units to ensure we provide opportunities for donation, where possible, to be included in the care of families facing the death of a child.
Donation after Neurological Determination of Death
The AoMRC guidance document should be used to determine the death by neurological criteria in > 2months post term.
In April 2015 guidance was released for determination of death by neurological criteria by the RCPCH. This guidance relates specifically to infants from 37 weeks gestational age (including corrected gestational age) to 2 months post term.
Donors aged less than 18 by donor type, 1 April 2013 – 31 March 2023
Donation from infants with antenatal diagnosis of life limiting abnormalities
There have been cases where babies diagnosed with anencephaly and other life limiting conditions have been able to donate organs and tissues following their death. However, this remains a rare event and the likelihood of donation occurring under these circumstances is small. Further guidance has been given from the UK Donation Ethics Committee which can be found below.
For the most current information on supporting families in decisions regarding donation where there is a diagnosis antenatally of a life limiting illness please consult section 7 of the OTDT Paediatric Manual (PDF 1.3MB). Alternatively, you can contact the Specialist Nurse Team on 03000 20 30 40.
Other resources
Donation in Infants and Neonates
Organ and Tissue donation opportunities from small infants and neonates should be considered as a usual part of end of life care, but always in conjunction with advice from the specialist nurse team to ensure families are only offered options that are realistic. For further BAPM endorsed guidance you can download the following document, Guidance and information to support Neonatal Units (PDF 288KB).
In April 2015 guidance was published by the Royal College of Paediatric and Child Health on the determination of death by neurological criteria in infants from 37 weeks corrected gestational age to 2 months post term. This guidance has the potential to increase the possibility of greater options for transplantation from these patients.
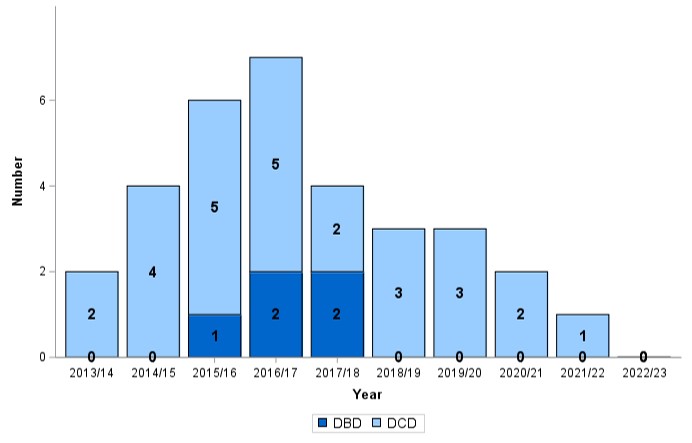
Donors aged less than 6 months by donor type, 1 April 2013 – 31 March 2023
Paediatric Donor Optimisation
In addition to ensuring the opportunity for donation is offered in all cases where it is possible we need to consider the focus of treatment following neurological determination of death. The focus changes from life saving to the optimisation of organs for transplantation. We have a commitment to provide the highest number of organs in the best possible condition through optimisation of donor physiology.
The principles of optimization are unchanged from adults but specific consideration for paediatric patients and paediatric practice is important. Local protocols which are agreed with clinical, nursing and pharmacy staff are important to ensure optimization objectives are clearly met.
Please follow the link for the optimisation care bundle (83KB) for use on patients >37 weeks CGA - 15 years. The cardiothoracic SCOUT project phase 2 does not apply to patients under 16 years of age.
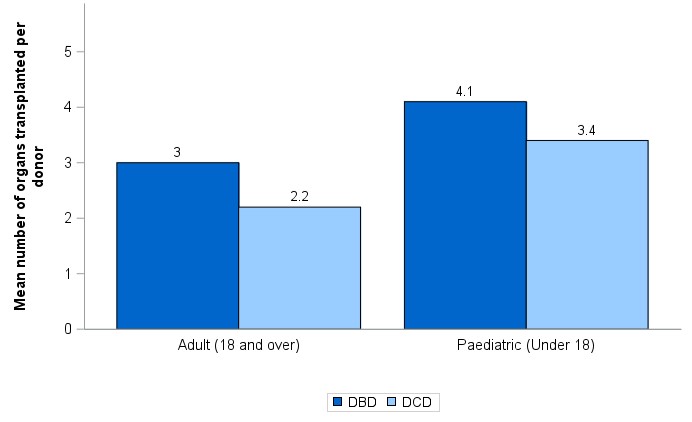
Mean number of organs transplanted per donor by age group and donor type, 1 April 2022 – 31 March 2023